This Is How Excess Glucose Damages Your Cell Powerhouses, Causing Disease
Glucose is essential for human health as it is the only energy source for the liver and red blood cells and the preferred energy source for many other cells in the body, particularly the brain. Excess glucose intake, however, can lead to metabolic disorders such as insulin resistance and type 2 diabetes.
Scientists have theorised that these metabolic disorders are caused by cellular dysfunction, and until recently, haven’t established the pathways causing cellular dysfunction.
A new study in mice now reveals that excess glucose reduces the amount of polyunsaturated fatty acids in mitochondrial cell membranes, negatively affecting their integrity and functionality and ultimately causing cell dysfunction and damage.
The study “Excess dietary carbohydrate affects mitochondrial integrity as observed in brown adipose tissue,” was published in Cell Reports.
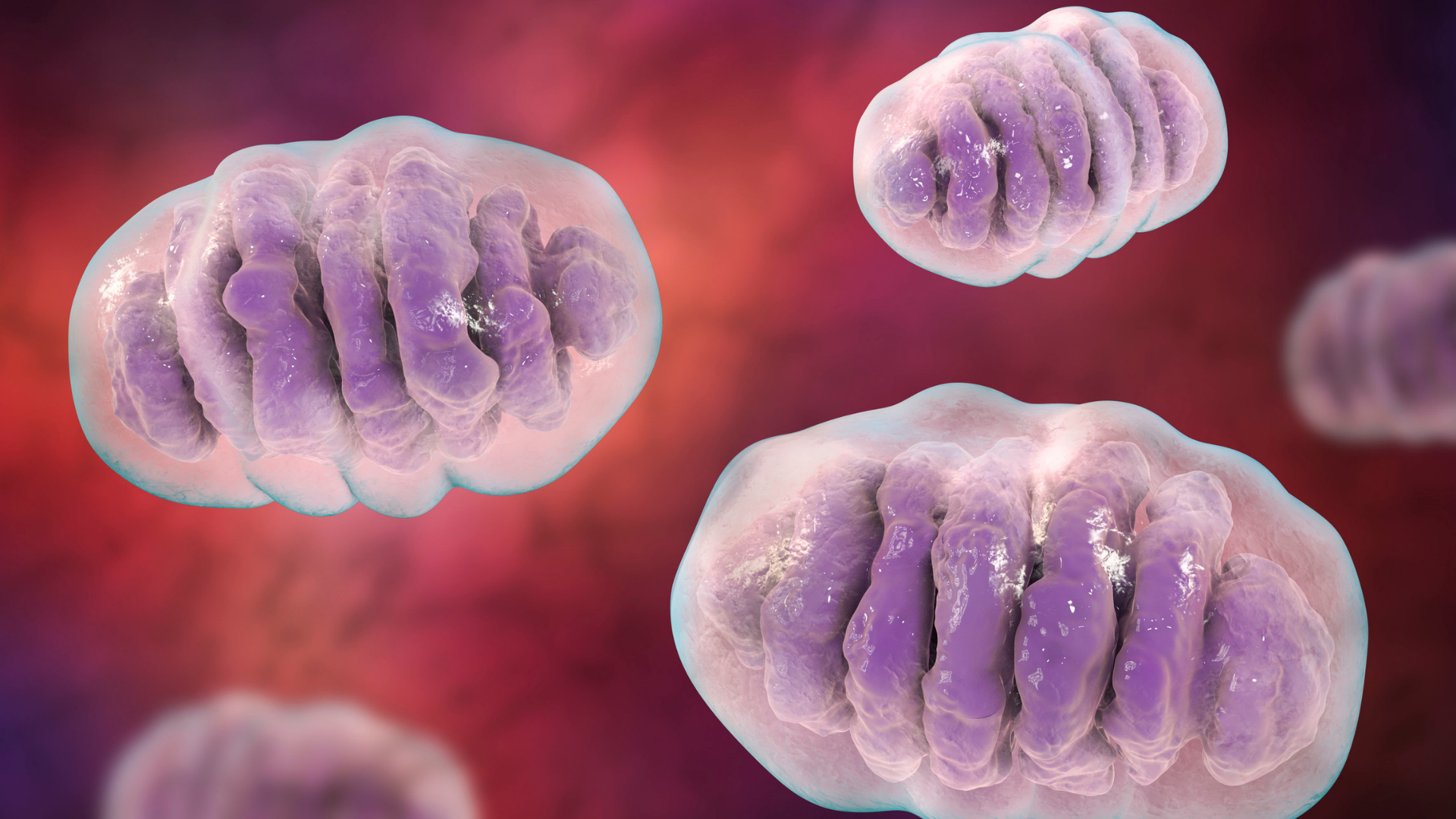
Mitochondria – the cell’s powerhouses – are crucial for optimal cell functioning. They produce energy and remove damaging free radicals from cells and tissue. Mitochondrial defects are implicated in many health conditions, including cardiovascular disease, cancer and nerve disorders.
Brown adipose tissue (BAT) is a fat tissue that converts energy from food into heat. It contains many mitochondria, which it depends on to keep the body warm, particularly during cold temperatures.
Glucose uptake by cells is regulated by a protein called thioredoxin-interacting protein (TXNIP). TXNIP is usually bound to glucose transporter (GLUT) proteins. When cells need glucose, TXNIP dissociates from GLUT proteins allowing glucose to enter the cells in a controlled manner. However, when TXNIP is absent or dysfunctional, excess glucose flows freely into cells, causing cells to store excess glucose as fat.
To study the effects of excess glucose intake on mitochondrial functioning, a team of researchers at the Van Andel Institute in the United States studied BAT mitochondria in mice lacking TXNIP.
The researchers initially compared BAT from mice containing TXNIP (wildtype, WT) with those lacking it (knockout, KO) and found that BAT from KO mice was paler than WT due to higher fat content.
To determine if KO BAT could be activated appropriately to produce heat in cold temperatures, KO and WT mice were subjected to 4ºC for 4 hours. Both mice responded adequately to cold temperatures by burning fat for heat. However, KO mice were less effective at generating heat. KO mitochondria were also significantly swollen, with broken inner membranes (cristae) after cold temperatures. Interestingly, the swelling was reversed once the mice were fed very low carbohydrate (ketogenic) diets for five weeks.
Proper mitochondria functioning is dependent on the fatty acids present in its cell membrane. Mitochondria need long-chain polyunsaturated fatty acids (PUFAs), and a particular form of lipid called cardiolipin to retain its shape, functionality and flexibility.
Considering the critical role of PUFAs in mitochondria functionality, the researchers investigated the genes regulating long-chain PUFA production and the long-chain PUFA content of mitochondria in WT and KO. Compared to the WT mice, KO mice had significantly decreased expression of five genes necessary for long-chain PUFA production. KO mice also produced lower quantities of long-chain PUFAs required for mitochondria shape and flexibility. However, once fed a ketogenic diet, KO mice increased expression of the five PUFA genes to similar levels in WT mice.
“The body needs sugar, or glucose to survive, but, as the saying goes, ‘all good things in moderation,” Ning Wu, assistant professor at Van Andel Institute said in a press release. “…Too much glucose in cells, which is directly linked to the amount of sugar consumed in one’s diet, affects lipid composition throughout the body, which in turn affects the integrity of mitochondria. The overall effect is a loss of optimal function,” she added.
Ultimately, the study shows a clear early link between excess carbohydrate intake and mitochondrial function, confirming the detrimental consequences of a high-sugar diet.
“Although we may not always notice the difference in mitochondrial performance right away, our bodies do,” Wu said. “If the lipid balance is thrown off for long enough, we may begin to feel subtle changes, such as tiring more quickly. While our study does not offer medical recommendations, it does illuminate the early stages of metabolic disease and provides insights that may shape future prevention and therapeutic efforts,” she added.

